News Story
Maisel to Investigate Little-Known Organ in the Body

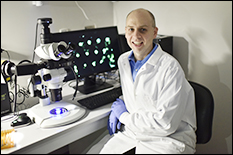
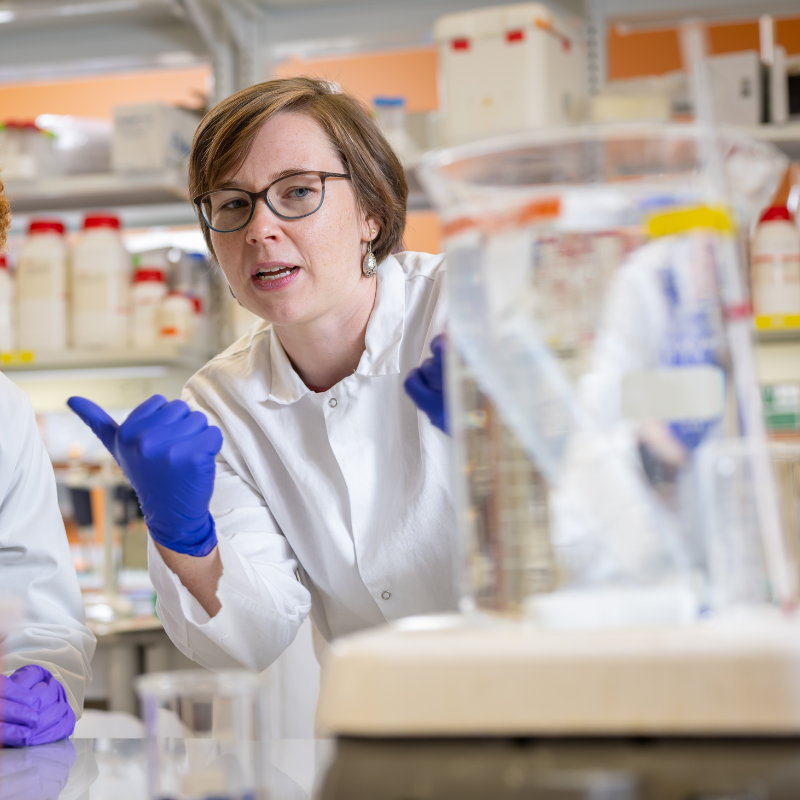
Dr. Katharina Maisel
Scientists – including those who specialize in the field of drug delivery – still know surprisingly little about a part of the human body that likely impacts the effectiveness of therapeutics used to treat or prevent a variety of diseases.
But, Fischell Department of Bioengineering (BIOE) Assistant Professor Katharina Maisel hopes that will soon change, thanks in part to her lab’s most recent undertaking.
In the human body, the interstitium, or interstitial tissue – composed of connective tissue cells, water, and other elements – makes up a supporting framework located outside the blood and lymphatic vessels and organs. In recent years, scientists have posited that the tissues and fluid-filled spaces that comprise the interstitium as well as the lymphatic and blood vasculature – and that carry cells and molecules throughout the body – likely influence how cancers and other diseases spread.
Recognizing this, Maisel is working to develop new techniques to study the interstitium and lymphatics so that bioengineers can one day design therapeutics to be both more effective in combating disease and less harmful to the body’s healthy cells. Maisel was awarded a five-year, $1.8 million grant from the National Institute of General Medical Sciences of the National Institutes of Health to support these efforts.
“It’s both fascinating and surprising that the scientific community still has so much to learn about the spaces that surround cells within a tissue, given that these spaces make up such a large part of the body,” Maisel said. “But, we have ample reason to believe that the interstitium plays a part in how diseases progress.”
Interstitial fluid resembles blood plasma. It occupies the space that surrounds cells in the body and carries nutrients and cell waste products. When this fluid reaches lymphatic vessels found widely throughout the body, it takes on the role of “lymph” and is carried to the lymph nodes, the body’s immune system command center.
Because interstitial tissue governs what exactly enters the lymphatic vessels, Maisel and her team believe that advanced understanding of interstitium and lymphatic transport could one day empower bioengineers to design more effective therapeutics for a range of diseases.
“Systemic delivery of therapeutics throughout the body works well for the treatment of certain health challenges. But, the reality is that most diseases and cancers would respond best to therapeutics that are designed to target a specific site in the body – such as the site of an infection or tumor,” Maisel said. “To best target therapeutics to a specific site or cell, we need to design them in a way that they can cross tissue spaces to travel away from where they are administered – such as an injection site – and toward their intended target. Similarly, we can take advantage of natural processes – like lymphatic transport – that shuttle materials toward potential target sites like the lymph nodes. Targeting lymphatic transport processes can play a critical role in modulating the body’s immune response.”
When studying lymphatic transport, bioengineers like Maisel have to consider a unique feature of lymphatic vessel physiology: lymphatic vessels typically rest in a collapsed – or closed – state until they are pushed open by interstitial fluid flow into the vessel. This means that it’s interstitial fluid flow that drives molecules and particles – which could include viruses or, conversely, nanoparticles containing therapeutics – into lymphatic vessels.
But, scientists and bioengineers have very limited understanding of how different factors – such as interstitial flow or inflammation – actually affect lymphatic transport of molecules and particles. One of the reasons for this knowledge gap is that lymphatic vessels are buried deep within tissues. To make matters more difficult, lymph fluid is clear and difficult to detect.
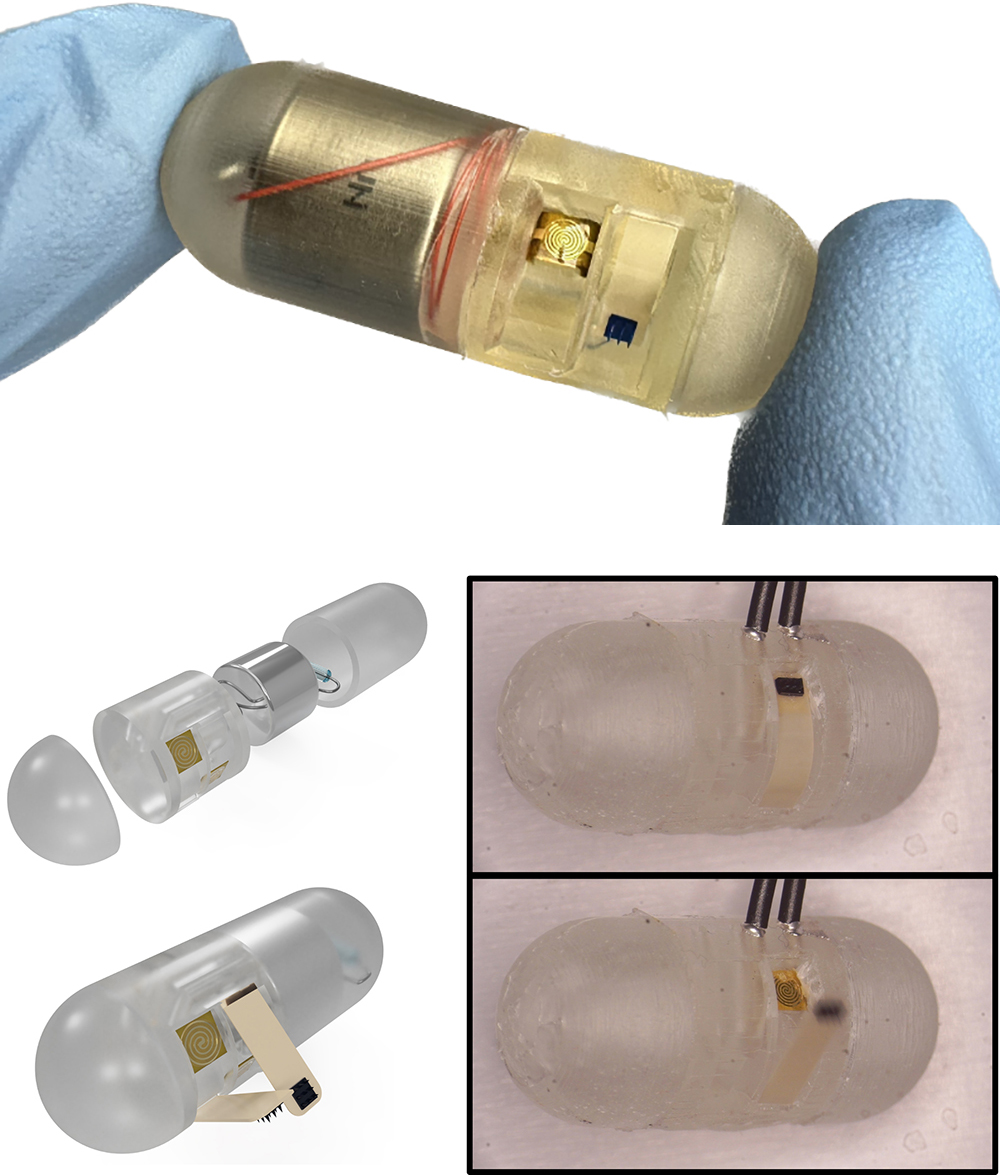
Recognizing this, Maisel and her lab aim to build 3D microfluidic lymphatic vessel models that incorporate interstitial flow, allowing the team to visualize and monitor lymphatic transport of materials, proteins, and particulates in an entirely new way. Maisel’s team is also working with BIOE Associate Professor Alisa Clyne and members of her Vascular Kinetics Lab to develop microfluidics techniques that will help make this possible.
“By designing in vitro model systems of lymphatics, we can address specific questions about how transport is regulated in healthy tissues and how this may be modulated in disease,” Maisel said. “We also hope to gain a better understanding of how disease and inflammation affect interstitial tissue spaces and integrity using our ex vivo model systems.”
In addition, Maisel and her team plan to use a specialized technique to examine living interstitial tissue slices, allowing the group to examine the structure of the interstitium in a way no one ever has. Rebecca Pompano, an associate professor of chemistry and biomedical engineering at the University of Virginia, and members of Pompano’s lab first developed this technique for immune tissues and used it to measure the diffusion of active proteins through live lymph node tissue.
Moving forward, Maisel’s group will work to investigate how physiological processes shape interstitial tissue spaces. Their goal is to steer the design of therapeutics to pass through interstitial tissue barriers in order to reach key targets in the body.
“Improving our basic understanding of lymphatics and the interstitium can help guide our design of how to best deliver therapeutics in health and disease,” Maisel said. “Chronic inflammatory diseases like inflammatory bowel disease and allergies, in particular, require us to think about solutions that won't affect patients’ overall immune functions or cause significant systemic side effects. Additionally, learning more about the interstitium and lymphatics may also guide new drugs to modulate interstitial tissue and lymphatic functions when they are disrupted in disease states. We are excited to receive this NIH NIGMS funding in order to pursue these avenues in my lab.”
This research is supported by a grant from the National Institute of General Medical Sciences of the National Institutes of Health. In addition to Clyne and Pompano, BIOE Associate Professor Kim Stroka (Ph.D. ‘11) and members of her Cell and Microenvironment Lab will contribute expertise to this work.
Published August 5, 2021