News Story
Cuff, Scale, and Smartphone
Checking your blood pressure on a regular basis is an essential part of measuring your health. Often this involves a conventional cuff device that estimates blood pressure from an oscillometric pressure waveform using population average methods.
New research by Jin-Oh Hahn, an assistant professor in the department of mechanical engineering at the University of Maryland, in collaboration with Ramakrishna Mukkamala at the Michigan State University and Omer Inan at the Georgia Institute of Technology, is paving a way toward new affordable, ultra-convenient, and patient-specific approaches to monitor blood pressure and cardiovascular risk predictors.
The Super Cuff
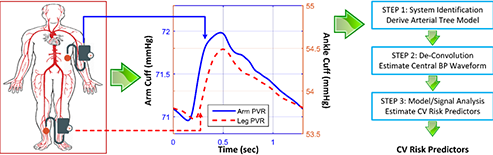
The "super cuff" is a suite of algorithmic technologies Hahn and his colleague Mukkamala are developing to advance the capability of conventional blood pressure cuff devices by enabling the monitoring of advanced cardiovascular risk predictors as well as traditionally measured brachial blood pressure.
"It is based on the conventional cuff," explains Hahn, "but the algorithms inside of it can adapt blood pressure and cardiovascular risk predictor computations to individual subjects and potentially improve the accuracy of the readings."

According to Hahn, who recently published a paper on the topic, the patient-specific algorithms in the super cuff may enable more accurate automatic cuff blood pressure measurement in patients with large artery stiffening while limiting the number of required cuff inflations or deflations per measurement, as well as monitor cardiovascular risk predictors whose measurement used to necessitate expensive equipment and trained operators.
In "Patient-Specific Oscillometric Blood Pressure Measurement: Validation for Accuracy and Repeatability" published in IEEE Journal of Translational Engineering in Health and Medicine, Hahn and Mukkamala point out that unlike conventional population average methods, which use the same parameter values in their empirical method for transforming the oscillogram to blood pressure levels in all patients, the new method determines the parameter values for each patient at the time of measurement to improve the accuracy of blood pressure monitoring.
"Accuracy can be maintained over a wider blood pressure range," explains Hahn. "By using a physiological model, the method could be more robust to oscillogram differences caused by respiration and variability in heart rate."
The Scale
In an effort to improve the tracking of blood pressure in individual subjects, Hahn, in collaboration with Mukkamala and Inan, has also pursued research to assess the capabilities of a weighing scale-like system to calculate pulse transit time through larger and more elastic arteries by measuring ballistocardiography and foot photoplethysmography waveforms.
"Using the scale to measure your blood pressure is completely passive," says Hahn. "We don't require the user to do anything. You stand on it and that's it. This ease of use is very appealing."
The scale is equipped with sensors that measure the subject's small-amplitude vertical movement that occurs in response to an ejection of blood from the heart. "Each ejection of blood by the heart causes movement of the body," explains Hahn. "Although this amplitude is very small, we can measure it and translate that signal into a blood pressure reading."
Hahn and his colleagues found that the weighing scale-based pulse transit time is a better marker of blood pressure than conventional pulse arrival time widely being pursued. Their work involved measuring the scale pulse transit time, conventional pulse arrival time, and cuff blood pressure in humans during interventions that increased blood pressure but changed the pre-ejection period and smooth muscle contraction differently. While the scale pulse transit time tracked diastolic blood pressure changes well, the conventional pulse arrival time was significantly inferior in tracking these changes.
"Scale pulse transit time also tracked systolic blood pressure changes better than conventional pulse arrival time, but not to an acceptable level," Hahn notes. "We hope that with more development, scale pulse transit time will produce a convenient and reliable measurement of blood pressure."
More recently, Hahn and his colleagues also found that blood pressure may be monitored solely based on the ballistocardiography measurement alone. Based on a rigorous mathematical modeling analysis, Hahn and his colleagues discovered the physical mechanism underlying the genesis of ballistocardiography and showed that ballistocardiography morphology is closely associated with blood pressure waves in the aorta.
"Ballistocardiography measurement may provide surrogate measures of diastolic and pulse (systolic - diastolic) pressures, which may enable independent monitoring of diastolic and systolic pressures from the ballistocardiography measurement alone," Hahn observes.
The Smartphone
Since convenience is a big factor, Hahn also worked with Mukkamala in developing a smartphone-based system that can conveniently measure blood pressure. The idea is to allow people to check their blood pressure anytime and anywhere.
"We came up with a system including a smartphone encasing and an app that is simple enough to use to evaluate the validity of our idea," says Hahn. "We demonstrated that it is certainly feasible to check your blood pressure with a smartphone. This convenience allows people to check their blood pressure as often as they like, wherever they are."

The technology is activated when the user presses a finger against the smartphone and the external pressure of the underlying artery is steadily increased. The smartphone then measures the applied pressure and resulting variable amplitude blood volume oscillations. To guide the amount of external pressure applied over time through the finger pressing, users receive visual feedback from the smartphone, which computes systolic and diastolic blood pressure from the measurements.
"It certainly has room for improvement," Hahn recognizes, "but we think the ubiquitous benefits of this technology could really serve to improve hypertension management."
Published April 20, 2018